Stroke – An Overview
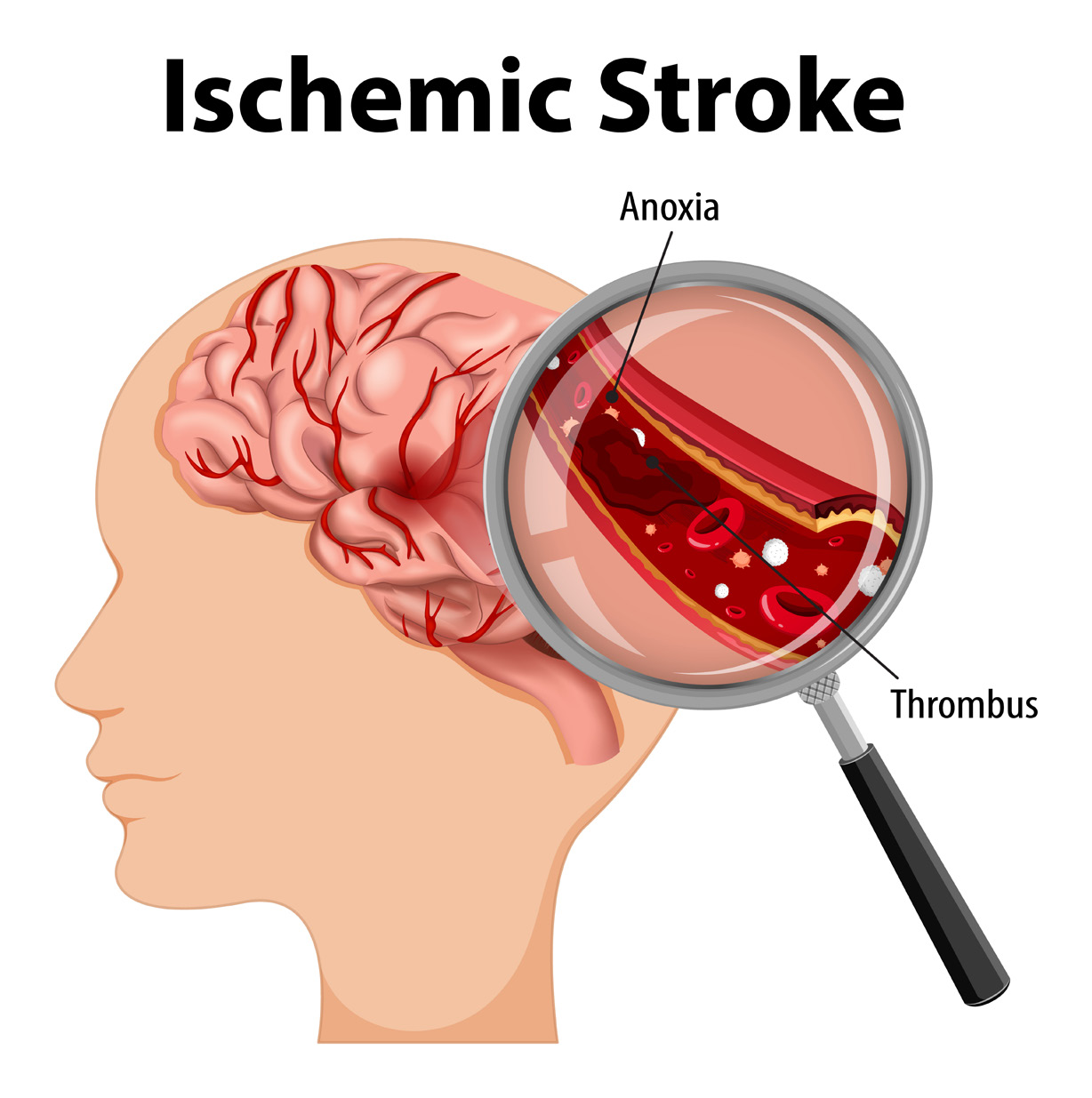
Ischemic stroke is characterised by the sudden loss of blood circulation to an area of the brain, resulting in acorresponding loss of neurologic function. Acute ischemic stroke is caused by thrombotic or embolic occlusion of a cerebral artery and is more common than hemorrhagic stroke (bleeding in the brain).
Stroke is the leading cause of disability and the fifth leading cause of death Epidemiologic studies indicate that 82–92% of strokes are ischemic. According to the World Health Organisation (WHO), 15 million people suffer stroke worldwide each year. Of these, 5 million die, and another 5 million are left permanently disabled.
A focused medical history for patients with ischemic stroke aims to identify risk factors for atherosclerotic and cardiac disease, including the following:
- Hypertension
- Diabetes mellitus
- Tobacco use
- High cholesterol
- History of coronary artery disease, coronary artery bypass, or atrial fibrillation
Stroke should be considered in any patient presenting with an acute neurologic deficit (focal or global) or altered level of consciousness. No historical feature distinguishes ischemic from hemorrhagic stroke, although nausea, vomiting, headache, and a sudden change in the patient’s level of consciousness are more common in hemorrhagic strokes.
- Hemiparesis, monoparesis, or (rarely) quadriparesis
- Hemisensory deficits / Dysarthria
- Facial droop
- Ataxia
Emergent brain imaging is essential for excluding mimics (SAH, ICH, masses) and potentially confirming the diagnosis of ischemic stroke. Non-contrast CT scanning is the most commonly used form of neuroimaging in the acute evaluation of patients with apparent acute stroke. Magnetic resonance imaging (MRI) with angiography (MRA) has been a major advance in the neuroimaging of stroke. Digital subtraction angiography is considered the definitive method for demonstrating vascular lesions, including occlusions, stenoses, dissections, and aneurysms.
The central goal of therapy in acute ischemic stroke is to preserve tissue in the ischemic penumbra, where the perfusion is decreased but sufficient to stave off infarction. Tissue in this area of oligemia (less blood supply) can be preserved by restoring blood flow to the compromised area and optimizing collateral flow.
Recanalization strategies, including the administration of intravenous (IV) recombinant tissue-type plasminogen activator (rt-PA) and intra-arterial approaches, attempt to establish revascularization so that cells in the penumbra can be rescued before irreversible injury occurs. Restoring blood flow can mitigate the effects of ischemia only if performed quickly. Medical management with antiplatelet and statin therapy with help of physiotherapy and rehabilitation can transform the treatment part.
Palliative care is also an important component of comprehensive stroke care.



