Wet and Distraught A medical wake up call

Enuresis or bedwetting is a common problem in children and often neglected due to multiple reasons. Parents, caregivers and sometimes even primary care physicians do not give it the appropriate attention due to the popular belief that the child will grow out of it.
The International Children’s Continence Society recommends that a 6-year-old child with enuresis must be offered treatment, and at an earlier age if the child desires to be dry. Untreated, enuresis gives rise to low self-esteem in the child, hinders participation in activities like camps and stay overs giving rise to feelings of isolation; it also causes significant distress to the parents. Additionally, some enuretics go on to be adults with enuresis (prevalence 0.5- 1% adults).
Factors implicated in the pathogenesis of primary enuresis are, singly or a combination, a small bladder capacity, high arousal threshold from sleep and low nocturnal anti diuretic hormone (ADH) secretion, resulting in nocturnal polyuria. Associated co-morbid factors that have been identified in children with bedwetting are constipation, sleep disordered breathing, obesity and behavioral disorders like ADHD or autism spectrum disorder.
Enuresis may be associated with daytime symptoms like voiding postponement, where the child may adopt postures like crossing the legs or sitting with heels at the perineum to delay voiding. Other symptoms may be urgency, increased frequency and daytime incontinence. Children who have daytime symptoms are said to have non-monosymptomatic enuresis in contrast to those who have isolated bedwetting or monosymptomatic enuresis. Evaluation of these children is based on history to establish whether enuresis is monosymptomatic or non-monosymptomatic and to identify co morbid factors.
Step one in the management of bedwetting is urotherapy. This encompasses demystification: explaining to the family regarding the proposed pathogenesis of enuresis, removing any shame the child may be suffering, imagining that bedwetting was her/ his fault and alleviating the guilt of the parents who believe that it is a result of their poor child rearing skills. The child is advised to drink about 6 glasses of fluids in a day and most of it during the daytime and early evening, to void every 2 ½ -3 hours, ensure one soft bowel movement in a day, both in the correct posture. The child and parents are asked to maintain a voiding diary to understand the bladder capacity as well as for the family to register the problem. Daytime symptoms are usually addressed first. Comorbid conditions also need to be managed early or concomitantly with the management of enuresis. Parents need to understand that waking up the child to void every night keeps him dry only for that night, however does not contribute to ‘training’ towards a dry bed.
Specific treatments for monosymptomatic enuresis are alarm therapy and desmopressin. An alarm is a bell that goes off in response to the activation of a moisture-sensitive sensor placed in the child’s underwear when she/he sleeps. This works on the principle of conditioning so that the child finally learns to wake up to the sensation of a full bladder. The alarm has the lowest relapse rate. Desmopressin, a vasopressin analogue available as a melt tab, is ideal for children with nocturnal polyuria as demonstrated on the voiding diary. It is also very useful for short periods for camps and stay-overs. The two may be used in combination if one is not effective. The anticholinergic drug oxybutynin may be added to desmopressin especially when there is some bladder overactivity.
The key to successful management of enuresis lies in developing a rapport with the enuretic child and working with the family as a team towards a shared goal of achieving dryness when asleep and hence ensuring a better quality of life.
Paediatric Renal Service, Renal Unit, KEMH
POEM - Singing praises in treatment of Motility Disorders
The motility disorders are on the rise due to improved diagnostic modalities but therapeutic treatment armada has made strikingly large strides in recent years predominantly via endoscopic route. The commonly encountered disorders on day-to-day practise are Achalasia Cardia, Distal Esophageal Spasm and Hirschsprung disease. In this short review we will focus on esophageal motility disorders and treatment modalities.
Esophageal Motility Disorders These disorders are defined as an esophageal disease attributable to neuromuscular dysfunction that causes symptoms referable to the esophagus, most commonly dysphagia, chest pain, or heartburn. Using this definition, there are only 3 firmly established primary esophageal motility disorders: Achalasia, Distal Esophageal Spasm (DES), and GERD.
Esophageal motility disorders can also be secondary phenomena, in which case esophageal dysfunction is part of a more global disease, such as in Pseudo achalasia, Chagas disease, and PSS (scleroderma).
Major And Minor Disorders of Esophageal Motility
All this disorders and their patterns are diagnosed on High Resolution Esophageal Manometry (HRM). The latest classification has classified the disorders in two broad categories. The previously classified Major disorders are now reclassified as Disorders of EGJ outflow while minor disorders have been reclassified as Disorders of Peristalsis. Here is latest Chicago V4 classification for esophageal motility disorders.
| CLASSIFICATION | DISORDER | DEFINITION |
|---|---|---|
| Disorders of EGJ Outflow (Major Disorders) | Type I Achalasia | Abnormal median IRP & 100% failed peristalsis |
| Type II Achalasia | Abnormal median IRP, 100% failed peristalsis, & ≥20% swallows with Pan-esophageal pressurization | |
| Type III Achalasia | Abnormal median IRP & ≥20% swallows with premature/spastic contraction and no evidence of obstruction | |
| EGJ Outflow Obstruction | Abnormal median IRP and not meeting criteria for achalasia | |
| Disorders of Peristalsis (Minor Disorders) | Absent Contractility | Normal median IRP & 100% failed peristalsis |
| Distal Esophageal Spasm | Normal median IRP & ≥20% swallows with premature/spastic contraction | |
| Hypercontractile Esophagus | Normal median IRP & ≥20% hypercontractile swallows | |
| Ineffective Esophageal Motility | Normal median IRP, with >70% ineffective swallows or ≥50% failed peristalsis |
The degree of ganglion cell loss parallels the duration of disease, likely progressing from EGJ outflow obstruction to type II achalasia, to type I achalasia, to end-stage achalasia. Type III achalasia seems to have a unique pathogenesis, characterized by myenteric plexus inflammation and altered function, but not destruction.
Clinical Features
1. Dysphagia- All patients have solid food dysphagia; the majority of patients have variable degrees of liquid dysphagia. The onset of dysphagia is usually gradual and progressive. Dysphagia is sensitive to temperature of food; some cases may report improved symptoms with hot food. Dysphagia also gets relieved with repetitive swallows or changing position or Valsalva manoeuvres.
2. Regurgitation- With long-standing disease, there is progressive esophageal dilatation, and regurgitation becomes frequent with recumbency. The regurgitant is often recognized as food that has been eaten hours, or even days, previously. It tends to be nonbilious, non-acid, and mixed with copious amounts of saliva.
3. Chest pain- Early in the course of achalasia, approximately two thirds of patient’s complaints of chest pain. Its aetiology is unknown, but is thought to be related to the occurrence of esophageal spasm
4. Other symptoms- Hiccups, Halitosis, weight loss, and aspiration pneumonia. Nearly 10% of cases have bronchopulmonary complications as a result of regurgitation and aspiration. Another fortunately rare, symptom of achalasia is airway compromise and stridor because of the dilated esophagus compressing the membranous trachea in neck.
Diagnostic Modalities
1. Endoscopy- First test for evaluating new onset dysphagia, because it combines the ability to detect most structural causes of dysphagia with the ability to obtain biopsies.
2. Commonly seen findings on endoscopy are dilated esophagus, tertiary contractions, retained food and liquid particles in esophagus and resistance in negotiating scope beyond GE Junction.
3. Contrast Imaging- Modified barium swallow is imaging of choice. The common findings are, dilated esophagus, spastic contractions, delayed barium passage and incomplete relaxation of GE Junction.
4. High Resolution Manometry- This is a test in which intraluminal pressure sensors are positioned within the esophagus to measure the contractile characteristics of the esophagus and segregate it into functional regions. The Chicago classification uses standardized parameters such as Median IRP (Integrated Relaxation Pressure), DL (Distal Latency) and DCI (Distal Contractile Integral). On behalf of this parameters and contractile pattern the disorders of motility have been classified. (Refer to Table 1)
5. Intraluminal impedance measurement- predominantly used for GERD
6. FLIP (Functional Lumen Imaging Probe)
Treatment Modalities
1. Pharmacologic Therapy
Amyl nitrite, Sublingual Nitroglycerin, Theophylline, and β2-adrenergic agonists have also been tried, with variable success.
2. Surgical Therapy
Heller Myotomy- Published series of the efficacy of Heller myotomy in treating achalasia report good to excellent results in 62% to 100% of patients, with persistent dysphagia in fewer than 10%. The risk of reflux symptoms is more severe compared to other modalities.
3. Endoscopic Therapy i) Botulinum Toxin Injection- Landmark study of botulinum toxin in achalasia reported that intra-sphincteric injection of botulinum toxin decreased LES pressure by 33% and improved dysphagia in 66% of patients for a 6-month period. This modality has been preferred in frail patients who are not candidate for surgical or endoscopic myotomy.
ii) Pneumatic Dilation- Rigiflex dilators which are long, noncompliant, cylindrical balloons with radio opaque markers are used. They are designed to be passed over a guidewire and positioned across the LES fluoroscopically. The clinical efficacy reported for dilation ranges widely from 32% to 98%. It is considered as initial treatment modality in patients of type II achalasia cardia. Ballon dilation should only be considered in patients who are surgical candidates because it carries 1-5% risk of perforation.
iii) POEM (Per Oral Endoscopic Myotomy)
PER ORAL ENDOSCOPIC MYOTOMY (POEM)
Different types-
1. POEM- Achalasia cardia (Anterior or Posterior approach)
2. G POEM- Gastroparesis
3. Z POEM- Zenker’s Diverticulum
4. D POEM- Esophageal Diverticulum
5. PREM- Per Rectal Endoscopic Myotomy for Hirschsprung disease.
CASE Recently POEM for Achalasia Type II was performed in KEMH. A 33-year-old
gentleman presented with classical symptoms of Dysphagia for solids and liquids, weight
loss of 5-6 Kg and reflux symptoms since past 1 year. On evaluation, UGI scopy showed dilated esophagus and tertiary contraction with resistance for passage of scope through GE junction. High Resolution Manometry showed raised Median IRP (26.6 mmHg) with absence of peristalsis and Pan-esophageal pressurization. PROCEDURE Important steps of this procedures are highlighted below with the help of images for easier understanding.
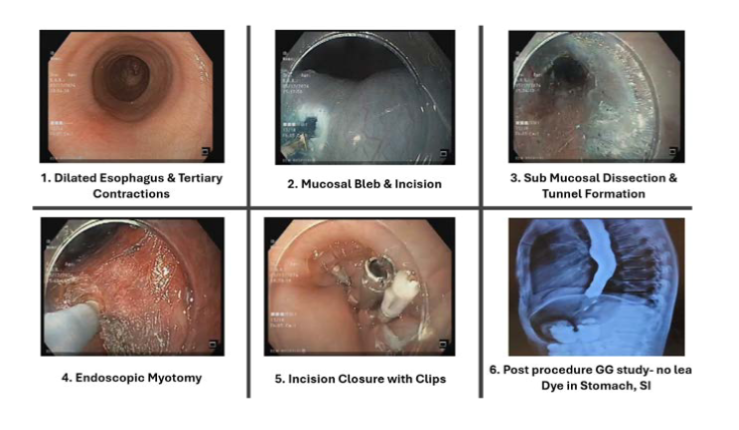
The total duration of procedure was under 75 mins. No immediate post procedure complication was noted. On POD-1, Gastrograffin swallow was performed which did not show any leak and dye could easily be passed in stomach, small bowel. He was started on diet with in 24 hours of procedure and discharged within 48 hours procedure. On follow up after 15 days (POD-17), patient is tolerating normal diet and started gaining some weight.
WHATS DATA ON EFFICACY OF POEM
Latest data by North et al in 2023 compared POEM vs Hellers vs Pneumatic Dilatation. The conclusion was, POEM has improved efficacy compared to PD and Hellers myotomy with similar cost-effectiveness. POEM results showed comparable patient outcomes with laparoscopic myotomy. Overall, POEM is a feasible first-line treatment for achalasia.
TREATMENT OPTIONS FOR OTHER MAJOR MOTILITY DISORDERS
1. Psuoachalasia- underlying cause such as malignancy, lymphoma should be managed.
2. Distal Esophageal Spasm- POEM
3. Hypercontractile esophagus/ Jack Hammer esophagus- CCB, Nitrate Trial or POEM
4. Absent peristalsis- No established data, may be managed with PPI/ Pro-kinetics
CONCLUSION
POEM have been recent effective answer for questions thrown by most of the motility disorders. Different types of POEM’s are being performed according to underlying aetiology such as Achalasia, Gastroparesis, Zenkers and Esophageal diverticulum.
So, to briefly summarise-“The swansong of POEM has just begun and long it may sing.”




