Epilepsy in children
Bridging the Gaps in Treatment: Part 2
Swaraj, a four-year-old boy came to the Epilepsy Clinic with multiple (almost daily) uncontrolled seizures. Despite initial resistance from his parents, thorough investigations were carried out, leading to a confirmed diagnosis of epilepsy. Swaraj was promptly started on anti-epileptic medication, and his parents were counselled and educated about medical care and seizure management.
Thanks to the collaborative efforts of the neurologist and developmental psychologist Swaraj's co-morbid learning difficulty was also addressed. Regular follow-up visits allowed us to assess his progress in the medical, academic, and social domains-and helped his parents understand and adjust to a chronic disorder like epilepsy.
Swaraj's story highlights the importance of early intervention, medication compliance, and a holistic multidisciplinary approach to managing paediatric epilepsy, ultimately providing hope for a brighter future for these young patients.

Successful management of paediatric epilepsy is not a simple, one-stop solution but rather a complex and ongoing journey. It requires the collaborative efforts of doctors, caregivers, healthcare infrastructure, family and social support. Epilepsy management involves a multidisciplinary approach, where neurologists, developmental psychologists, physical therapists and other specialists work together to provide comprehensive care to achieve optimum outcomes.
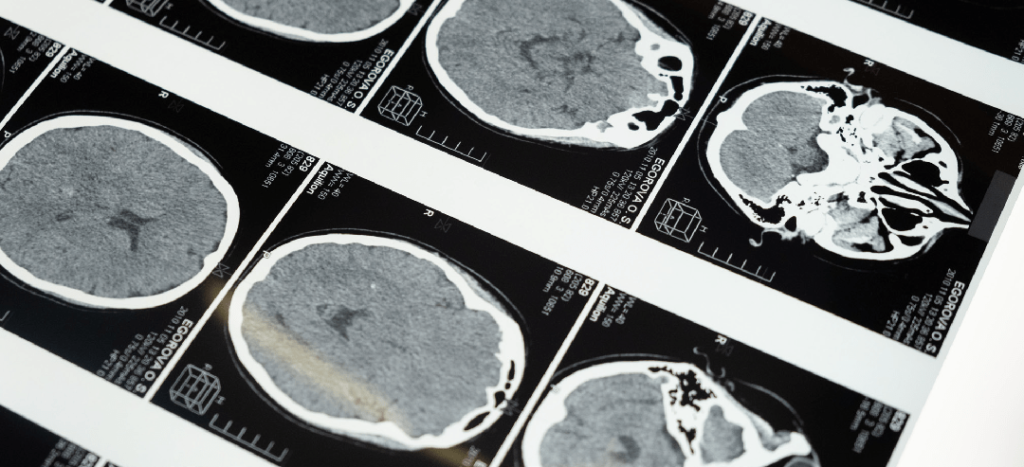
The journey begins with accurate diagnosis and treatment initiation. Doctors carefully evaluate the child's medical history, conduct various tests usually an EEG examination, some blood tests, and MRI/CT scans, and tailor a treatment plan that includes anti-epilepticmedications. It is crucial for caregivers and families to understand the importance of medication compliance, proper dosage, and potential side effects as well.
Compliance refers to the extent to which individuals with epilepsy, or parents of children with epilepsy, adhere to the physician's instructions regarding how and when to take the prescribed medication, as well as any recommended lifestyle modifications. Compliance holds particular significance in epilepsy treatment due to the potential risk of seizures if the medication's blood levels drop too low. Poor adherence to medication regimens has long been recognized as a major factor contributing to treatment failures in epilepsy, presenting an ongoing challenge in achieving the essential therapeutic goal of seizure control.
Open communication, education about the medication's purpose and potential side effects, and strategies for integrating medication into daily routines- such as use of calendars; utilising reminder alarms in watches or mobile phones; using cues (medicine placed near a toothbrush to aid the morning and evening dose), can contribute to improved compliance rates.
Beyond medication, epilepsy management requires a supportive healthcare infrastructure. This includes regular follow-up visits, where doctors assess the child's progress, adjust the treatment plan if needed, and provide guidance and counselling to caregivers. Access to specialized clinics, diagnostic facilities, and trained healthcare professionals is vital to ensure optimal care.
It is well known however that Epilepsy services are currently largely limited to urban areas, leaving rural communities with insufficient access to specialized healthcare and facilities. To address this issue and improve accessibility, a public health approach model can be implemented using existing healthcare infrastructure. The immediate focus could be on capacity building of healthcare providers, utilizing appropriate diagnostic technology, and ensuring a consistent supply of epilepsy medications.
Several approaches have begun to be employed by India and other developing countries to deliver epilepsy services in rural areas. These include the fixed satellite clinic model- where apex institutions establish clinics in remote locations, the camp approach where specialists or trained physicians conduct rural camps, the mobile clinic approach involving a single visit by a neurologist, and the rural approach which integrates epilepsy care into primary healthcare services.
Additionally, training general practitioners in epilepsy care, involving key informants such as school teachers and community leaders in identification and education, utilizing community health workers for identification, referral, and follow-up, and implementing a communitybased rehabilitation model could be beneficial. Thus helping bridge the gap in healthcare accessibility and ensuring better care.
Further, complementary therapies are sometimes considered as additional approaches to traditional treatments. One such therapy that has gained attention is the ketogenic diet (modified Atkin's diet). The ketogenic diet is a high-fat, low-carbohydrate, and low-protein diet that aims to alter the chemical balance in the brain, potentially reducing the likelihood of seizures. Particularly for children with seizures that are not effectively controlled by antiepileptic medications, research has shown a potential reduction in the frequency of seizures in some children. It is important to note that the ketogenic diet should only be undertaken under the supervision of an epilepsy specialist and with the guidance of a dietitian to ensure proper implementation and monitoring.
Epilepsy surgery may be an option when medicines don't control seizures. This is a condition known as medically refractory epilepsy or drug-resistant epilepsy. Epilepsy surgery is done to stop seizures or limit their severity. Surgery also is done to lessen seizure-related deaths, decrease the use of anti-seizure medications and decrease the possible side effects of the medicines.
Equally important to medical treatment is the role of family and social support. Epilepsy can have a significant impact on the child's daily life, education, and social interactions. Families need to provide a nurturing environment, address any learning difficulties or developmental challenges, and encourage adherence to medication and healthy lifestyle habits.
Unfortunately, misconceptions and stigma surrounding epilepsy present significant challenges for individuals and families affected by the condition. Numerous studies highlight the persistent lack of public understanding about seizures and epilepsy.
Addressing this issue requires educational initiatives targeted at individuals with epilepsy, their families, and the wider community. Such efforts are crucial in reducing stigma, which, in turn, can contribute to improved diagnosis and treatment outcomes.
Public awareness campaigns, mnemonic devices, street-play models, audio-visual communication channels and comprehensive epilepsy education programs in schools and educational institutions are effective strategies for increasing understanding and dispelling misconceptions. Support groups and community organizations can offer additional guidance, share experiences, and provide emotional support for both the child and their caregivers.
The provision of counselling services for patients and their families at healthcare institutions is also essential. These sessions play a vital role in promoting acceptance, building resilience, and preventing the dissemination of misinformation and incorrect practices related to epilepsy management. Support Groups and other social welfare organisations can aid families with adjustment and understanding of the disorder as well.
At the individual level the journey of managing paediatric epilepsy is filled with ups and downs, successes and challenges. It requires ongoing collaboration, communication, and teamwork between doctors, caregivers, healthcare infrastructure systems, and the child's support network. By working together, this collective effort can help improve the quality of life for children with epilepsy, empowering them to thrive and reach their full potential.
At the country level- Epilepsy remains a significant public health challenge in India, characterized by stigma, socioeconomic disparities, a large treatment gap, and a deficient healthcare system. Addressing this issue requires a multidisciplinary approach involving neurologists, public health professionals, psychiatrists, psychiatric social workers, psychiatric nurses, and program managers. A comprehensive public health response is needed, encompassing prevention, improved care, and rehabilitation- which is sustainable, cost-effective, and integrated into existing programs. Key elements include service delivery, capacity building, integration, mobilization of public support, and increased awareness.
By adopting this integrated public health model, India can effectively address the burden and impact of epilepsy while ensuring holistic care and support for individuals living with the condition and help bring out the best in them.



