Tunneled Cuff Catheter
Tunneled cuffed catheter (TCC) is a form of long-term vascular access for hemodialysis of CKD patients. It is a 19 – 23 cm long tube with 2 lumens placed in a neck vein with its tip in right side of heart. Unlike temporary catheter, tube of TCC passes under the skin for 8-10
cm. and comes out over chest. It is called as tunneling of catheter. TCC is usually inserted under fluoroscopy guidance in Cathlab to assure accurate placement.
TCC has 2 major advantages over a temporary dialysis catheter. First, the chance of transmission of infection along the skin exit site is reduced significantly as it has a cuff in the tunnel which excites fibrosis. Second, the catheter gets firmly attached to skin which
prevents its dislodgement. Compared to AV Fistula, TCC can be used immediately after placement while AV Fistula takes 4-6 weeks for maturation and TCC doesn’t need needle pricks for every dialysis session.
The most common complication associated with TCC is catheter related blood stream infection (CRBSI). The chance of CRBSI can be minimized by meticulous catheter care as per protocol.
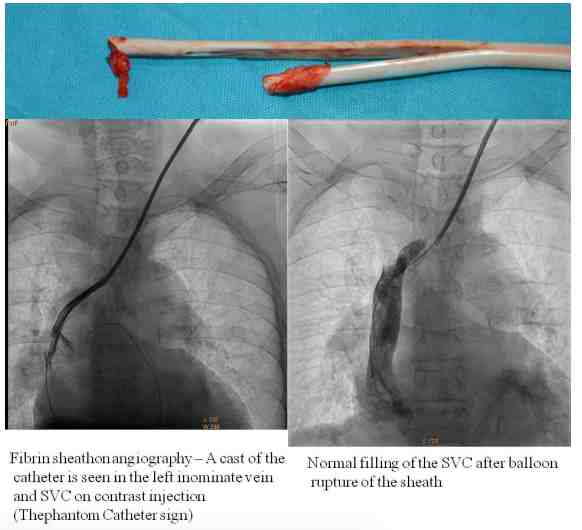
Sometimes TCC can malfunction due to obstruction by blood clot in lumen or a sheath formation around its tip causing ball valve obstruction. These complications need special treatment / interventions. Hence AV Fistula is still the first choice of vascular access for maintenance hemodialysis and TCC is indicated in patients where creation of AV Fistula is not possible.



